|
|
Post by sportsrancho on Nov 18, 2022 17:20:02 GMT -5
Facebook is having glitches and I can’t get into my Vdex account.. this is so extremely annoying to me I can’t even tell you.
If you wanna write the questions down I’ll ask Bill, he’s traveling right now … but what I do know is that we bill Medicare for our diabetic care, and we have for years. $35 for Afrezza like Peppy says it’s a different recent change. And free CGM’s….!!! Did I read that right? Since we basically have had to eat the cost so our patients could each have one this is a very good thing😎👍🏻
|
|
|
|
Post by peppy on Nov 18, 2022 17:34:26 GMT -5
Facebook is having glitches and I can’t get into my Vdex account.. this is so extremely annoying to me I can’t even tell you. If you wanna write the questions down I’ll ask Bill, he’s traveling right now … but what I do know is that we bill Medicare for our diabetic care, and we have for years. $35 for Afrezza like Peppy says it’s a different recent change. And free CGM’s….!!! Did I read that right? Since we basically have had to eat the cost so our patients could each have one this is a very good thing😎👍🏻 Bill as best MNKD pro-boards can determine, Medicare covering insulin for $35 passed under the inflation protection act. Mike C said, "In 2023, we fully expect that Afrezza will be covered in Medicare at $35 under the inflation protection act bill that was passed. That changes the game as one of the major objections for Afrezza is around access," What do you think this legislation means for Afrezza and Vdex business? Sayhey said, " Afrezza is available in every (2023) plan I checked. I even checked Peppy's and 100% its there. The banner is pretty clear $35 per month on 60 and 90 day prescriptions. " |
|
|
|
Post by peppy on Nov 18, 2022 18:12:10 GMT -5
I think that verbiage about having to cover each form is from the Affordable Insulin Now Act which is dead. My feeling is that the devil is in the detail and I would wait to see how it gets handled next year. I have tried reading the relevant sections (Sec. 11406, 11408) a couple of times and am not sure I really understand this. They refer to covered insulin products (in-formulary), but it's not clear to me that insurers can be compelled to add inhaled insulin. There is a reference in Sec. 11408, which is a safe harbor clause to protect people from getting their health plan reclassified by the IRS if the insurer doesn't offer all formats I believe (I am NOT a lawyer to be clear!) Aged - have you gone to Medicare.gov and checked? Afrezza is available in every plan I checked. I even checked Peppy's and 100% its there. The banner is pretty clear $35 per month on 60 and 90 day prescriptions. Lets give Mike credit, what he said was correct. I don't know how they did it but they got the language into the legislation. I guess because Kindle wanted it for ALL Americans and Medicare was the compromise. Dan Kindle introduced the Affordable Insulin Now Act. Kildee introduced and passed it through the House in March 2022 with support from Republicans and Democrats. As a part of the passage of the Inflation Reduction Act, Senate Republicans blocked Kildee’s legislation to cap insulin prices for all Americans from becoming law. While Kildee was still able to successfully cap the price of insulin at $35 for seniors on Medicare in the Inflation Reduction Act, his bill, the Affordable Insulin Now Act, would cap insulin prices for all Americans at $35 a month. Here is what the ADA says "To make sure seniors are getting these savings right away, people who are charged more than $35 per month for their insulin in the first few months after the new Medicare copay cap is enacted will be reimbursed." diabetes.org/sites/default/files/2022-08/What-People-with-Diabetes-Need-to-Know-about-the-Inflation-Reduction-Act.pdfHere is how it got born in the Inflation Reduction Act www.kff.org/medicare/issue-brief/explaining-the-prescription-drug-provisions-in-the-inflation-reduction-act/#:~:text=The%20Inflation%20Reduction%20Act%20limits,and%20no%20deductible%20will%20apply. wow, good work Sayhey, thank you. |
|
|
|
Post by nylefty on Nov 18, 2022 18:18:45 GMT -5
www.kff.org/medicare Under the new Inflation Reduction Act requirement, all Part D plans do not have to cover all insulin products at the $35 monthly copayment amount, only those insulin products that are covered on a plan’s formulary.
|
|
|
|
Post by peppy on Nov 18, 2022 18:30:50 GMT -5
www.kff.org/medicare Under the new Inflation Reduction Act requirement, all Part D plans do not have to cover all insulin products at the $35 monthly copayment amount, only those insulin products that are covered on a plan’s formulary.
Afrezza was on silver scripts plan. YEARLY DRUG & PREMIUM COST $6,188.76 I think I am paying 6 dollars a month for the plan. SilverScript SmartSaver (PDP) Aetna Medicare | Plan ID: S5601-181-0 Star rating: 3.5 stars MONTHLY PREMIUM $5.20 Includes: Only drug coverage YEARLY DRUG & PREMIUM COST $6,188.76 Retail pharmacy: Estimated total drug + premium cost $6,188.72 Mail-order pharmacy: Estimated total drug + premium cost |
|
|
|
Post by nylefty on Nov 18, 2022 20:43:22 GMT -5
Facebook is having glitches and I can’t get into my Vdex account.. this is so extremely annoying to me I can’t even tell you. If you wanna write the questions down I’ll ask Bill, he’s traveling right now … but what I do know is that we bill Medicare for our diabetic care, and we have for years. $35 for Afrezza like Peppy says it’s a different recent change. And free CGM’s….!!! Did I read that right? Since we basically have had to eat the cost so our patients could each have one this is a very good thing😎👍🏻 CGMs are not free, although Medicare may pay 80 percent of the cost.
Medicare covers therapeutic continuous glucose monitors as durable medical equipment (DME). You will be responsible for your Medicare Part B deductible and 20 percent of the Medicare-approved cost. Medicare will cover the other 80 percent after you meet your deductible. |
|
|
|
Post by oldfishtowner on Nov 18, 2022 20:54:17 GMT -5
www.kff.org/medicare Under the new Inflation Reduction Act requirement, all Part D plans do not have to cover all insulin products at the $35 monthly copayment amount, only those insulin products that are covered on a plan’s formulary.
If it is not in a patient's Part D plan's formulary, MNKD should tell the patients to switch to a plan for 2024 that does and in the meantime either provide the drug free or provide a coupon to bring the cost down to $35/month. If enough patients switch to plans that cover Afrezza in their formulary, the rest will get the message pretty quickly.
Complaining to your Congressman as sayhey suggests is good, but also get the AARP to do something as well. It doesn't hurt to have a strong lobbyist on your side.
|
|
|
|
Post by sportsrancho on Nov 18, 2022 22:29:58 GMT -5
Peppy…
Vdex…
People don’t leave us if we can’t get their insurance to cover Afrezza… we just get them on something else and try the best we can to control their blood sugar, but as far as telehealth goes those people are specifically wanting a script for Afrezza so I would think it would help immensely.
|
|
|
|
Post by peppy on Nov 19, 2022 4:27:40 GMT -5
Peppy… Vdex… People don’t leave us if we can’t get their insurance to cover Afrezza… we just get them on something else and try the best we can to control their blood sugar, but as far as telehealth goes those people are specifically wanting a script for Afrezza so I would think it would help immensely.I'm going to go with immensely. Very interesting. MNKD share price + UTHR revenue + increase number of afrezza scripts and revenue = ad nauseam. I put a target on the monthly MNKD chart. 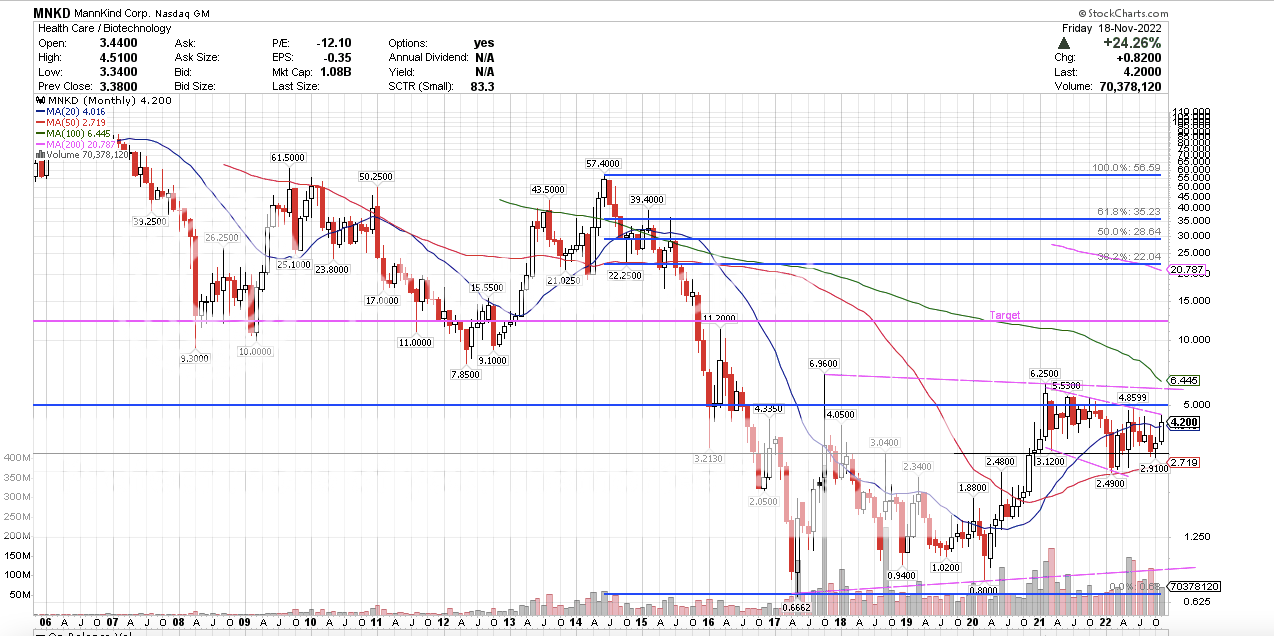 |
|
|
|
Post by sayhey24 on Nov 19, 2022 7:36:17 GMT -5
Facebook is having glitches and I can’t get into my Vdex account.. this is so extremely annoying to me I can’t even tell you. If you wanna write the questions down I’ll ask Bill, he’s traveling right now … but what I do know is that we bill Medicare for our diabetic care, and we have for years. $35 for Afrezza like Peppy says it’s a different recent change. And free CGM’s….!!! Did I read that right? Since we basically have had to eat the cost so our patients could each have one this is a very good thing😎👍🏻 CGMs are not free, although Medicare may pay 80 percent of the cost.
Medicare covers therapeutic continuous glucose monitors as durable medical equipment (DME). You will be responsible for your Medicare Part B deductible and 20 percent of the Medicare-approved cost. Medicare will cover the other 80 percent after you meet your deductible.As you say CGMs are covered under Part B. I think on this one I am going to let Abbott do the research for us as Part B coverage will vary by Advantage plan or supplemental coverage. Maybe Peppy can check with Aetna on her plan- you need to take insulin 3x per day which afrezza would qualify for Here is what Abbott is advertising "Medicare Covers the FreeStyle Libre System!" OK maybe its only 80%, IDK but lets see what Abbott says www.freestyle.abbott/us-en/medicare.html?utm_source=Google&utm_medium=SEM&utm_campaign=Brand&utm_content=Freestyle%20Medicare&gclid=EAIaIQobChMI9v2_laC6-wIVuf_jBx391AXdEAAYASAAEgK3ufD_BwE&gclsrc=aw.ds |
|
|
|
Post by agedhippie on Nov 19, 2022 10:19:17 GMT -5
Aged - have you gone to Medicare.gov and checked? Afrezza is available in every plan I checked. I even checked Peppy's and 100% its there. The banner is pretty clear $35 per month on 60 and 90 day prescriptions. Lets give Mike credit, what he said was correct. I don't know how they did it but they got the language into the legislation. I guess because Kindle wanted it for ALL Americans and Medicare was the compromise. ... The language in the legislation is exactly as I quoted it, I pulled that from the online copy of the act, and the IRS legislation. You have been quoting from articles that followed the bill being passed by the House, but before it was passed by the Senate The Senate changed a few things like removing the $35 limit for private insurance plans removed. You really need to look at the legislation itself, I gave you the relevant Sections to look at earlier. Meanwhile, Peppy will likely find that Afrezza is not covered for her since the IRA states covers in-formulary insulins and Afrezza is not in-formulary for Peppy's plan. Check here: ( www.aetnamedicare.com/en/prescription-drugs/check-medicare-drug-list.html). Not a covered insulin means it's full price. As I said earlier, the devil is in the detail. What Mike is talking about is that if you have a plan that covers Afrezza then you will will get it at $35, not that you can go to any insurer and demand Afrezza for $35. |
|
|
|
Post by peppy on Nov 19, 2022 11:46:14 GMT -5
Aged - have you gone to Medicare.gov and checked? Afrezza is available in every plan I checked. I even checked Peppy's and 100% its there. The banner is pretty clear $35 per month on 60 and 90 day prescriptions. Lets give Mike credit, what he said was correct. I don't know how they did it but they got the language into the legislation. I guess because Kindle wanted it for ALL Americans and Medicare was the compromise. ... The language in the legislation is exactly as I quoted it, I pulled that from the online copy of the act, and the IRS legislation. You have been quoting from articles that followed the bill being passed by the House, but before it was passed by the Senate The Senate changed a few things like removing the $35 limit for private insurance plans removed. You really need to look at the legislation itself, I gave you the relevant Sections to look at earlier. Meanwhile, Peppy will likely find that Afrezza is not covered for her since the IRA states covers in-formulary insulins and Afrezza is not in-formulary for Peppy's plan. Check here: ( www.aetnamedicare.com/en/prescription-drugs/check-medicare-drug-list.html). Not a covered insulin means it's full price. As I said earlier, the devil is in the detail. What Mike is talking about is that if you have a plan that covers Afrezza then you will will get it at $35, not that you can go to any insurer and demand Afrezza for $35. Meanwhile, Peppy will likely find that Afrezza is not covered for her since the IRA states covers in-formulary insulins and Afrezza is not in-formulary for Peppy's plan. Check here: (https://www.aetnamedicare.com/en/prescription-drugs/check-medicare-drug-list.html). Not a covered insulin means it's full price. As I said earlier, the devil is in the detail. Back to catch 22. sayhey24 .... you said $35 dollar insulin over the top of the page on the 2023 formulary.... and those words are no where to be found.... please explain? Just because a price comes up doesn't mean it is covered. Not much is covered on this plan but cheap generics. The cheap plan is just the cost of a bad tier system from my two minute attention span because I am not on any medications. The cost that came up, 1 30 day 4 unit pack. 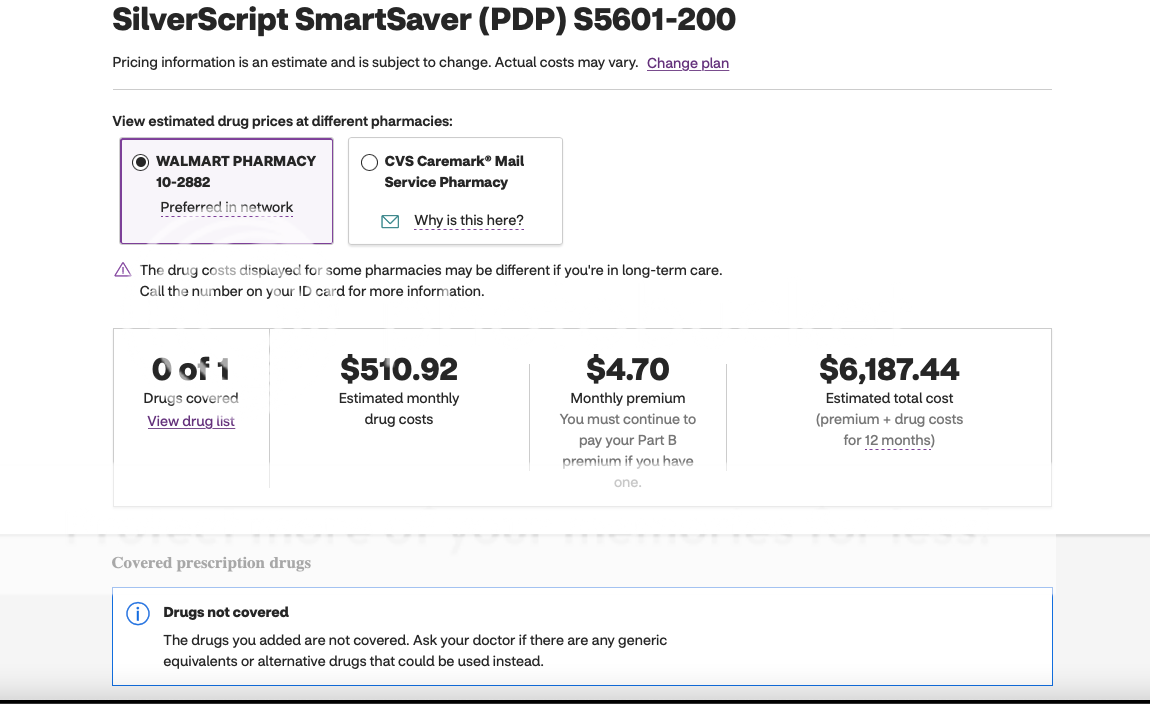 |
|
|
|
Post by sayhey24 on Nov 19, 2022 16:34:22 GMT -5
Aged - have you gone to Medicare.gov and checked? Afrezza is available in every plan I checked. I even checked Peppy's and 100% its there. The banner is pretty clear $35 per month on 60 and 90 day prescriptions. Lets give Mike credit, what he said was correct. I don't know how they did it but they got the language into the legislation. I guess because Kindle wanted it for ALL Americans and Medicare was the compromise. ... The language in the legislation is exactly as I quoted it, I pulled that from the online copy of the act, and the IRS legislation. You have been quoting from articles that followed the bill being passed by the House, but before it was passed by the Senate The Senate changed a few things like removing the $35 limit for private insurance plans removed. You really need to look at the legislation itself, I gave you the relevant Sections to look at earlier. Meanwhile, Peppy will likely find that Afrezza is not covered for her since the IRA states covers in-formulary insulins and Afrezza is not in-formulary for Peppy's plan. Check here: ( www.aetnamedicare.com/en/prescription-drugs/check-medicare-drug-list.html). Not a covered insulin means it's full price. As I said earlier, the devil is in the detail. What Mike is talking about is that if you have a plan that covers Afrezza then you will will get it at $35, not that you can go to any insurer and demand Afrezza for $35. Aged - Maybe I am wrong. Can you post a link to the legislation you are referring to. I see what you are saying but here is maybe whats going on - I think the issue is your link from Aetna is not reflecting the new legislation. Go to Medicare.gov and you will see afrezza. Medicare.gov does not reflect the 3 plans Aetna is showing on your link. It only shows one Aetna Plan D. In fact the one plan is not even on the Aetna site. However, it clearly lists afrezza on the details page on Medicare.gov and I see nothing about it being a non-covered drug as I see on the Aetna site. It clearly lists it and the details. I did not go through every plan but it is on every one I checked on Medicare.gov. Here is the banner from Medicare,gov "Important! Starting January 1, 2023, the cost of a one-month supply of each Part D-covered insulin will be capped at $35. If you get a 60- or 90-day supply of insulin, your costs can’t be more than $35 for each month’s supply of each covered insulin. This new $35 cap may not be reflected when you compare 2023 plans. You should talk to someone for help comparing plans." This is from Kildee's Official website - Dan Kildee introduced the Affordable Insulin Now Act. Kildee introduced and passed it through the House in March 2022 with support from Republicans and Democrats. As a part of the passage of the Inflation Reduction Act, Senate Republicans blocked Kildee’s legislation to cap insulin prices for all Americans from becoming law. While Kildee was still able to successfully cap the price of insulin at $35 for seniors on Medicare in the Inflation Reduction Act, his bill, the Affordable Insulin Now Act, would cap insulin prices for all Americans at $35 a month. Also remember we are not talking about private plans per say. I will go back and read the actual legislation Kildee got in there but I think they just lifted what he had in the Affordable Insulin Act. "Medicare's prescription drug benefit (Part D) is the part of Medicare that provides outpatient drug coverage. Part D is provided only through private insurance companies that have contracts with the federal government—it is never provided directly by the government". |
|
|
|
Post by nylefty on Nov 19, 2022 17:16:51 GMT -5
I find that the websites of health insurance companies are more credible when it comes to what drugs the companies cover than what the Medicare website says or seems to say.
|
|
|
|
Post by peppy on Nov 19, 2022 17:46:40 GMT -5
today in my mailbox from Aetna. Changes to the SilverScrip SmartSaver (PDP) 2023 Annual Notice of Change (ANOC) agedhippiesayhey24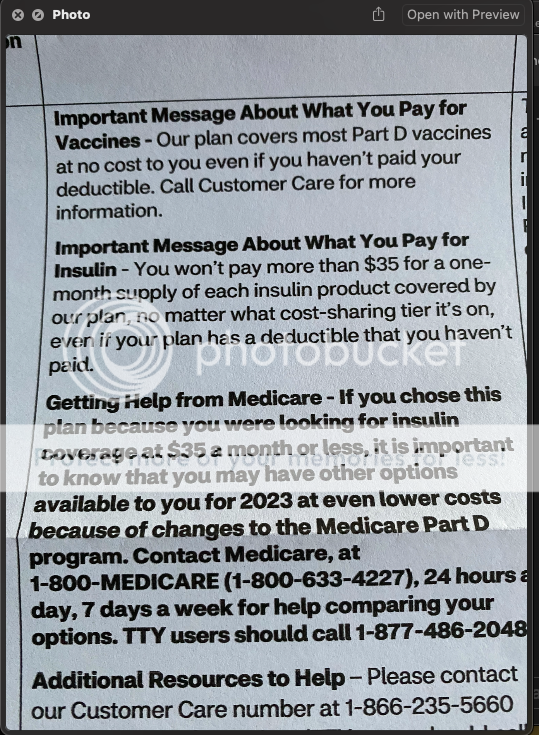 What do we think now? |
|